Introduction
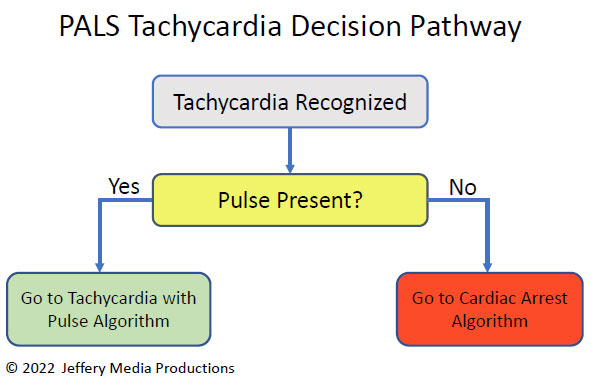
Tachycardia, defined as a heart rate greater than 100 beats per minute (BPM), is a common cardiac condition that can be either stable or unstable. The Advanced Cardiovascular Life Support (ACLS) tachycardia algorithm provides a structured approach to managing tachycardia based on patient stability, symptoms, and the underlying rhythm.
This article outlines the key steps in the ACLS tachycardia algorithm, including assessment, pharmacological interventions, and electrical therapies.
Step 1: Assess Patient Stability
The first step in managing tachycardia is determining whether the patient is stable or unstable.
Signs of Unstable Tachycardia
-
Hypotension (low blood pressure)
-
Altered mental status
-
Signs of shock (pale, cold, clammy skin)
-
Ischemic chest pain
-
Acute heart failure (pulmonary edema)
If the patient is unstable, immediate synchronized cardioversion is required.
Stable Tachycardia
If the patient is stable, proceed with further rhythm analysis to determine the type of tachycardia (narrow-complex vs. wide-complex).
Step 2: Identify the Type of Tachycardia
1. Narrow-Complex Tachycardia (QRS < 0.12 sec)
-
Typically supraventricular in origin (e.g., SVT, atrial fibrillation, atrial flutter).
-
Treatment depends on whether the rhythm is regular or irregular.
Regular Narrow-Complex Tachycardia (e.g., SVT)
-
Vagal maneuvers (e.g., carotid sinus massage, Valsalva maneuver).
-
If no response: Adenosine (6 mg rapid IV push, followed by 12 mg if needed).
Irregular Narrow-Complex Tachycardia (e.g., Atrial Fibrillation/Flutter)
-
Rate control with beta-blockers (e.g., metoprolol) or calcium channel blockers (e.g., diltiazem).
-
Consider anticoagulation if atrial fibrillation persists >48 hours.
2. Wide-Complex Tachycardia (QRS ≥ 0.12 sec)
-
Could be ventricular tachycardia (VT) or SVT with aberrancy.
-
If uncertain, treat as VT (more dangerous).
Stable Wide-Complex Tachycardia
-
Antiarrhythmics:
-
Amiodarone (150 mg IV over 10 min)
-
Procainamide (20-50 mg/min until arrhythmia suppressed)
-
Sotalol (100 mg IV over 5 min)
-
Unstable Wide-Complex Tachycardia
-
Immediate synchronized cardioversion (100-200 J monophasic or 50-100 J biphasic).
Step 3: Synchronized Cardioversion for Unstable Patients
-
Used for unstable SVT, atrial fibrillation/flutter, or VT with pulses.
-
Sedate the patient if possible.
-
Start with lower energy levels and increase as needed.
Step 4: Consider Underlying Causes
-
Electrolyte imbalances (hypokalemia, hypomagnesemia).
-
Myocardial ischemia/infarction.
-
Drug toxicity (e.g., digoxin, cocaine).
-
Hyperthyroidism.
Special Considerations
-
Polymorphic VT (Torsades de Pointes): Treat with magnesium sulfate (2 g IV) and correct underlying causes (e.g., prolonged QT).
-
Pulseless VT/VF: Follow ACLS cardiac arrest algorithm (immediate defibrillation).
Conclusion
The ACLS tachycardia algorithm provides a systematic approach to managing tachycardia based on patient stability and ECG findings. Key interventions include:
-
Unstable tachycardia → Immediate cardioversion
-
Stable narrow-complex → Vagal maneuvers, adenosine
-
Stable wide-complex → Antiarrhythmics (amiodarone, procainamide)
Rapid assessment and appropriate treatment improve outcomes in patients with tachycardia.
Visit our website: